Accounting vs. Billing Software: the Key Questions You Need to Ask
How to Record Accounts Receivable
These may be distinguished from notes receivable, which are debts created through formal legal instruments called promissory notes. Outstanding advances are part of accounts receivable if a company gets an order from its customers with payment terms agreed upon in advance. Since billing is done to claim the advances several times, this area of collectible is not reflected in accounts receivables.
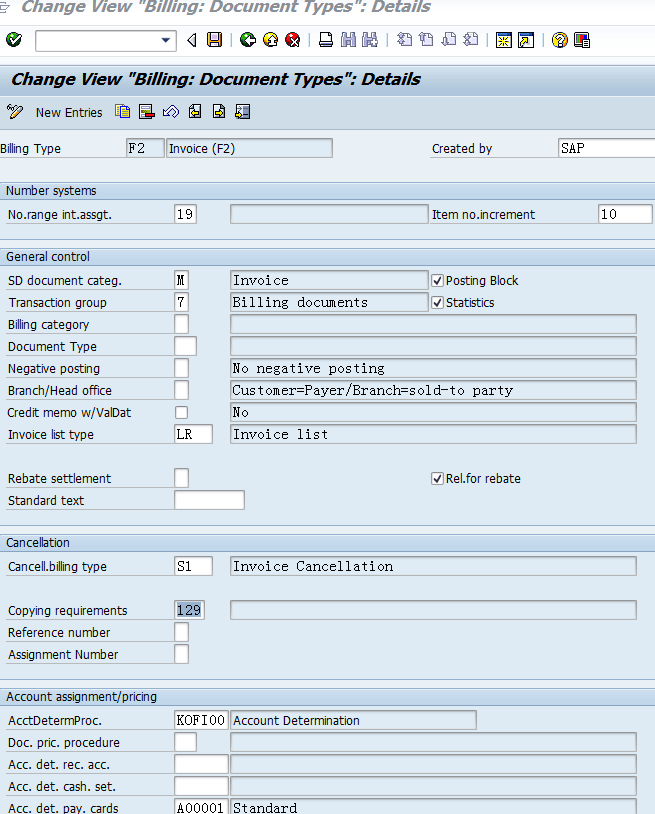
Formula to Calculate Billing & Invoice in SAP
The payment of accounts receivable can be protected either by a letter of credit or by Trade Credit Insurance. Communication with the payer (insurance company) and individual patients may be a long process.When the claim is approved, the healthcare provider will receive reimbursement for the services provided. The provider’s billing department will then attempt to recover the out of pocket expense from the patient. This is often done by sending invoices in the mail and manually calling the patient to remind them to pay their bill. Recovering patient out of pocket costs is increasingly becoming more important to providers as out of pocket costs have risen 37% since 2009. Once the payer has reviewed the claim, accepted it, and paid the agreed upon portion of services rendered, the provider now is ready to bill the patient.
What is the process of billing?
bill definition. An invoice or other document received from a vendor, supplier, etc. usually for goods or services received.
Recording a Bill Payable
When billing time arrives, patients are able to receive text messages, emails, phone calls, or even letters to notify them of pending payments. This avoids the need for collection agencies and allows the patient to pay with ease and based on their budget. Mobile banking and interest-free payment plans keep patients out of collections and enable providers to effectively recover past-due revenue. The first major form to be generated for medical billing is a superbill, also known as an encounter form.
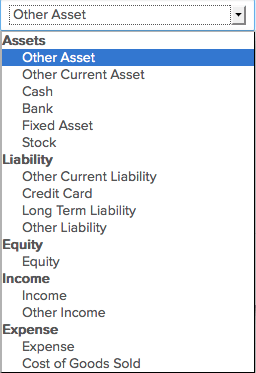
Accounts Receivable Models
With advanced machine learning, Enter’s AI can determine which communication format your customers prefer based on their demographics, knowing when to text, email, call, or send a letter on your behalf. With mobile banking and interest-free payment plans, collections can be made conveniently and regularly. This is something you’ll want to try to avoid, but it is one of the costs of doing business. If the customer from above never makes another payment, that means you did not receive $500 owed to you. You can pursue collections, but first, you’ll want to close it off your accounting books.This form is created by the medical coder after a patient has seen the doctor. The medical coder uses the information from the patient’s chart to note what diagnosis was made, what procedures were performed, what services or prescriptions were given, etc. Many practices have a preset list of common codes used by their physicians to speed up the coding process. The superbill is essential for reimbursement and must be accurately filled in before being submitted as a claim. The superbill must list the provider along with location of treatment and a signature with an NPI number.Therefore, it’s important for the medical biller to maintain healthy relationships with the patients. The goal of the medical biller to is make sure bills get paid, but not at the sacrifice of patient loyalty. Enter provides software to suit the needs of you and your patients from the start. Enter helps you to easily keep track of your customers, their balances, and payment history.In extreme cases, it may become necessary to turn the account over to a collections agency. Accounts receivable represents money owed by entities to the firm on the sale of products or services on credit.
What is an Invoice?
- Accounts receivable are legally enforceable claims for payment held by a business for goods supplied and/or services rendered that customers/clients have ordered but not paid for.
- It is one of a series of accounting transactions dealing with the billing of a customer for goods and services that the customer has ordered.
- These are generally in the form of invoices raised by a business and delivered to the customer for payment within an agreed time frame.
At the end of a set billing period, you will send an invoice to your customers detailing their account number, service or products used, the amount owed and payment due date. Billing and accounting software is available to help maintain this information.On every patient’s chart, the healthcare provider documents what services or procedures were performed and provides a diagnosis. That text is then translated into codes by a medical coder, each code indicating what was done or used by the physician and why. Next, a medical biller uses those codes, now called a superbill, to comprise a claim that will be sent to the patient’s insurance company.It can be difficult to collect on these types of bills if you are dealing with customers with bad credit, or who simply refuse payment. If you engage this kind of billing, consider offering discounts for prompt payment, but be prepared to assign staff to directly contact customers for outstanding bills.

You will issue credit memos to customers who paid for services or products they did not use or receive, or if an error in your billing caused the customer to overpay. Debit memos will be used in the opposite manner; when a customer uses more than his prepaid allowance, or if he is otherwise undercharged for his services. Debit memos essentially request more money from the customer, while credit memos, or credits, translate into money returned or service credits rolled over to the next billing cycle. For example, a landscaping company may mow a customer’s lawn, trim the hedges, and plant a few bushes.Accounts receivable are legally enforceable claims for payment held by a business for goods supplied and/or services rendered that customers/clients have ordered but not paid for. These are generally in the form of invoices raised by a business and delivered to the customer for payment within an agreed time frame. It is one of a series of accounting transactions dealing with the billing of a customer for goods and services that the customer has ordered.
Free Debits and Credits Cheat Sheet
Typically, whatever portion the insurance didn’t cover, the patient is responsible for. Medical billers are in charge of sending out the medical bills and following up with patients who have not paid. Each provider and facility has different guidelines regarding bill payments and contacting patients who are delinquent in their payments.Patient information must be complete, including demographics and insurance information. The very first step involves registering the patient, and obtaining their personal and insurance information. Based on a patient’s insurance plan, a medical biller can determine what services will be covered and which ones the patient will be responsible for, including co-payments. After the patient has checked out, a medical coder applies codes for the diagnosis and procedures performed, creating a superbill. From here the medical biller creates a claim including the cost of each procedure.
What does billing mean in accounting?
June 06, 2018. The following billing procedure addresses three tasks in the billing process, which involve collecting the information needed to construct an invoice, creating invoices, and issuing them to customers. Review Billing Information (Billing Clerk) Access the daily shipping log in the computer system.There’s a specific account, referred to as Bad Debt Expense which is used to record transactions that are the result of unpaid invoices. The Bad Debt Expense account is debited $500 and the Accounts Receivable account is credited $500. This removed the receivable out of your accounts and therefore doesn’t falsely inflate your total assets. Postpaid billing is a system in which the customer agrees to pay at a later date for products or services received.
Billing procedure
The medical biller must be careful to ensure that the claim is “clean” or is in compliance with state and federal regulations for coding and format. Some healthcare practices decide to even use a third party, known as a clearinghouse, to format claims according to the specifications of each insurance company and in accordance with HIPAA. It’s clear to see that one must be educated on the ins and outs of this process or it could easily result in a denied or rejected claim, which means no reimbursement. Credit and debit memos are not suitable as a sole billing system, but are important in case of changes to an account or payments, or errors made.A worst-case scenario may involve enlisting the help of a collection agency. From the start of a patient’s care, Enter determines what kind of communication the patient prefers based on machine learning and our AI’s recommendation.